Deadly diseases don’t wait. Neither should good ideas. So when two undergraduates thought they’d found a way to stop neurodegeneration, they took action.
After Phyl Gerber was diagnosed with amyotrophic lateral sclerosis in 2017, she went through stages of grief: anger, sadness, denial. Then her innate optimism kicked in.
“There was exciting research being done,” she recalls telling herself. “It all sounded so hopeful for the immediate future—I would be cured!”
ALS is a rare neurodegenerative disease that progressively robs patients of their ability to move, speak, eat, and breathe. Few people live longer than five years after diagnosis. When Gerber, 66, an athletic outdoorswoman all of her life—and a potter, gardener, wife, mother, and grandmother—learned of a six-month study for a new ALS drug, she “jumped on the opportunity to be a part of it.”
Gerber, of Amherst, MA, began taking the drug, AMX0035, in August 2017, and says that while her symptoms continued to progress, that progression slowed during the phase two, double-blind, placebo-controlled trial.
Thus when she learned, in December, that the study achieved its primary outcome—a statistically significant slowing of disease progression—she was “pleased but not surprised.” To the ALS world, though, the news was a revelation; the FDA has approved just two treatments for the disease, and there is no cure. Though the manufacturer, Cambridge, MA-based Amylyx Pharmaceuticals, wasn’t yet sharing data, any good news was cause to celebrate.
Perhaps even more surprising than an apparent success in this notoriously difficult field were the two people behind the new drug. Not yet 30 years old, they conceived of AMX0035 and founded Amylyx in 2013, when they were still undergraduates at Brown.
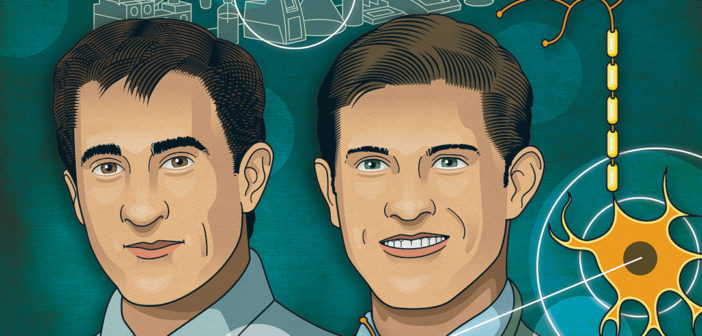
LIKE SO MANY TECH ORIGIN STORIES, the story of Amylyx begins in a dorm room. Justin Klee ’13 was just a few months shy of graduating with a neuroscience degree when he ran into his fraternity brother Josh Cohen ’14 late one night. Seven years later, Klee recalls that moment as they sit at the table in their spare, bright conference room in an East Cambridge office building: “Josh looked like he hadn’t slept in awhile.”
“I hadn’t.” Cohen chuckles. “That’s why.”
Cohen, 28, and Klee, 29, both have short dark hair, and are outgoing and affable. At Brown they played club tennis, and they worked in the lab of Christopher Moore, PhD, professor of neuroscience, learning to generate ideas, design experiments, analyze data, and question their results. Cohen, who was concentrating in biomedical engineering, had independently started reading journal articles on neurodegenerative diseases, “just following my curiosity,” when he hit upon an inspiration that robbed him of sleep: that two drugs, targeting two possible contributors to neuronal death, could be combined into one to slow the progression of neurodegenerative diseases like Alzheimer’s, Parkinson’s, and ALS.
The primary reason neurons die is one of the fundamental mysteries of these incredibly complex conditions. Some cases are genetic, but for many people, the cause of their disease is unknown. Cohen looked at what was going wrong after the process was triggered, focusing on two cellular organelles, the mitochondria and endoplasmic reticulum. Mitochondria produce energy and regulate cell death, or apoptosis; while the ER makes, folds, and transports proteins, and destroys proteins that are misfolded.
Cohen dug up small studies on two separate compounds that, in mouse models, seemed to protect against neurodegeneration and improve behavior and performance. Sodium phenylbutyrate (PB) stops neuronal death brought on by protein misfolding and accumulation. Tauroursodeoxycholic acid (TUDCA) inhibits mitochondrial stress and thus cell death.
Protein misfolding and accumulation have long been implicated in neurodegenerative diseases, though “it’s actually very hard for us to tell what goes wrong first,” says Anne Hart, PhD, professor of neuroscience at Brown. Hart, who isn’t affiliated with Amylyx, uses invertebrates to understand the mechanisms that cause neurodegeneration. “We know that toxic proteins are accumulating in patients,” she says. Targeting malfunctions in the mitochondria and ER is “a good strategy,” she adds, and combination therapy—which is used to treat many complex diseases, from cancer to HIV/AIDS to malaria—“makes sense because it gives you more than one way to help neurons deal with the disease.”
When the sleepless Cohen saw Klee that winter night seven years ago, he explained his theory: if PB and TUDCA were combined into one drug, together they might do an even better job of blocking the pathways in the mitochondria and ER that were killing neurons. “I thought what he was talking about sounded fascinating, and I started reading a lot about it,” Klee says. “The next day or something like that, we talked about it more, and decided to start a company.
“We smile looking back on that. What did that mean, starting a company?” he adds. “We really in retrospect knew absolutely nothing but—in a very Brown way—decided to just go and figure it out.”
Chris Moore, associate director of the Carney Institute for Brain Science, says that was “exactly the right impulse” to solve an urgent problem. “For some people it takes a lifetime to learn that that’s the secret sauce, the thing they need to do to change the field, to innovate, to change how we think about things: you need to do it,” he says. “They had a really good idea, and they were smart enough to know they should act on it.”
NEITHER OF THE FOUNDERS had aspirations of entrepreneurship when they came to Brown. Klee, who grew up in Waterford, CT, says he was “vaguely premed” and studied neuroscience because “it had a lot of creativity. There’s so little we know about the brain.” Cohen, a Canton, MA, native, wanted to work in pharmaceuticals. “I was interested and fascinated by new drugs, new therapies,” he says. “I didn’t necessarily want to found a company. … I just got hooked on an idea and didn’t want to let it go.”
By mid-March of 2013 they’d filed a provisional patent and incorporated Amylyx. It seemed like the fastest way to get their drug to patients. “When we first started, anybody who would listen, we would tell them that we were going to be in a clinical trial in three months, and no one could tell us otherwise, and we had answers for everything,” Klee says.
Reality stepped in quickly. Klee, the president of Amylyx, graduated and moved to Cambridge; Cohen, the CEO, spent as much time as he could at their shared workspace there while finishing his degree. They didn’t draw a salary for two years and took odd jobs, including clinical trial guinea pig, to get by. “We were pretty
broke,” Cohen says. “No other way to say it.”
Some of their earliest cheerleaders were at Brown, including Angus Kingon, PhD, the Barrett Hazeltine University Professor of Entrepreneurship and Organizational Studies and a professor of engineering; and Cohen’s senior-year roommate, Kent Leslie ’14 ScM’15. That year Leslie, a biology concentrator from Toronto who also wanted to work in pharmaceuticals, and Cohen talked about how to run Amylyx with just two people, “how you could work with toxicology consultants that aren’t on your payroll directly, but [have]30, 40 years’ experience. You can outsource all your experiments,” Leslie says.
Amylyx contracted with a lab in Finland to run their first experiment of the combination drug, AMX0035, in November 2013. Klee and Cohen funded it with their own savings, some money from their parents, and a grant that another early supporter, Alan Harlam, the founding director of the Social Innovation Initiative at Brown’s Swearer Center, helped them secure.
The in vitro study exposed rat neurons to hydrogen peroxide, which, Cohen says, has been shown to kill cells through the mitochondrial and ER pathways. “We found that either drug alone [PB or TUDCA] would rescue about 10 percent of the cells, but the combination would rescue about 100 percent of the cells,” he says. “That experiment was in essence the foundation of the company because it said that there’s something to hitting these two pathways simultaneously.”
Even as Klee and Cohen struggled to get investors, they found mentors among scientists and physicians. The initial target for AMX0035 was Alzheimer’s disease, and they landed meetings with a renowned Alzheimer’s researcher at Harvard, Rudolph Tanzi, PhD, and the former head of research at Pfizer, George Milne, PhD—two men who still play key roles as advisers. Klee says they had learned to turn their inexperience into an advantage: “What’s really nice when you’re young is that we could walk into a room and be dumb, and no one was surprised,” he says.
But Klee and Cohen got into the room because their idea was smart and their science was sound, their mentors say. Melanie Leitner ’93, PhD, a neuroscientist who advises organizations and investors who want to support research in the field, says their personalities further endeared the two founders. “Because they’re humble and willing to learn and willing to take input from anyone who would be willing to give them input … the network has really opened to them,” she says.
Kent Leslie, who was Amylyx’s first hire, as chief scientific officer, after he finished his master’s in biotechnology, adds: “Because we’re so young, we really didn’t have any preconceived notions of how to do any of these things. It’s allowed us to be very open to different advice.”
Amylyx followed the 2013 in vitro study with a successful trial in Alzheimer’s mouse models. But investors weren’t interested. At that time, Cohen says, there had been around “100 consecutive drug failures in Alzheimer’s. So coupling Alzheimer’s with two young founders is basically an investment people sprint away from.”
And so, like many startups, they pivoted. In 2015, they were visiting Tanzi at Massachusetts General Hospital when they had a chance meeting with Merit Cudkowicz, MD, MSc, P’20. “Merit is just a force of nature,” Klee says. The chief of neurology at Mass General and director of the Sean M. Healey & AMG Center for ALS, she had coincidentally led a small ALS trial of sodium phenylbutyrate six years earlier.
“They told me what they were doing,” Cudkowicz recalls, and she told them, “No, no, no, you’ve got to also work in ALS.” Her PB study had been stopped when they couldn’t get support for costly FDA-required animal toxicology studies. “So it’s super exciting to see it come back,” she says. “I was eager to help.”
With Cudkowicz on board, investors and ALS foundations were willing to back Amylyx. The unfortunate fact that the disease progresses so quickly also made their drug a sound investment. “The pitch we could ultimately make in ALS was that we could run a relatively short study with relatively few people for relatively low cost, and demonstrate a clinical effect,” Klee says, “whereas in Alzheimer’s, that was very difficult.”
IN ALS, THE MOTOR NEURONS, which run from the brain to the spinal cord and from there to the voluntary muscles, progressively degenerate and die. The brain loses control of voluntary movement, and the muscles atrophy. Because early symptoms of muscle weakness and stiffness may be similar to those of other diseases, an ALS diagnosis can take months and even years.
Phyl Gerber first knew something was wrong in the fall of 2015, when she began struggling to run up hills, and her bike rides got shorter and shorter. Many exams and tests and a year and half later, on the Ides of March, she got the diagnosis of ALS. Though she’s tried to remain positive, “the overall direction of the disease has been a slow, steady loss of physical abilities,” she says in an email that her husband of 46 years, John Gerber, PhD, typed for her.
Today Gerber must use a power wheelchair. She has limited use of just her right hand, and can no longer write or type. She has a feeding tube to take medications and get supplemental nutrition, and a noninvasive ventilator called a BiPAP to breathe more comfortably. The mask prevents her from speaking, heightening her sense of isolation. Though she uses a tablet and an “awkwardly” gripped stylus to convert typed words into an artificial voice, “It is unnatural and difficult to maintain a conversation,” she says. “But I’m glad to have it.”
The Gerbers believe things would be worse, though, without AMX0035. John, a professor of sustainable food and farming at the University of Massachusetts, charted his wife’s muscle strength measurements during and after the six-month trial, finding that her strength declined slowly during the study, then fell more quickly when it ended and she stopped taking the drug. Seven weeks later Gerber began taking it again when she enrolled in the open-label extension study, which Amylyx offered to all participants who completed the trial, including those on placebo. Again her symptoms abated; she’s still taking it twice a day. “We are convinced that my relatively slow progression has been largely due to my participation in this study,” she says.
“The goal [of the study] was to evaluate the safety, tolerability, biological activity, and clinical efficacy of the drug,” says Sabrina Paganoni, MD, PhD, the principal investigator and an assistant professor of physical medicine and rehabilitation at Harvard Medical School. The study used the best available functional rating scale for ALS to measure disease progression, and tracked muscle strength and respiratory function. “Because it was only six months in duration, we did not expect to see differences in survival,” Paganoni adds; the open-label extension study, which is ongoing, may provide that data.
Running a clinical trial was yet another area where the Amylyx team discovered, as Cohen says, “we knew nothing.” Paganoni, Cudkowicz, and other experts helped design the study, which enrolled 137 participants at 25 ALS centers across the country. The trial also measured biomarkers of neuronal degeneration and included a new way of assessing muscle strength.
“Justin and Josh really wanted to contribute to the field,” Cudkowicz says. She says they also improved recruitment using social media—an innovation she’s employing in another ALS trial that the Healey Center launched last fall—and solicited input from ALS patients and caregivers when they designed the trial, so that clinic visits wouldn’t be too exhausting for patients, and the endpoints would fit with clinicians’ standard practice. “That’s a nice thing about having new people in the field and new ideas,” Cudkowicz says. “They were very patient-centric, which is phenomenal.”
When the trial launched in June 2017, Cohen and Klee discovered a whole new level of responsibility. They’d get calls from site PIs about what to do when participants had to go to the hospital, or to decide whether to include people who didn’t really qualify. Though their chief medical officer, Patrick Yeramian, MD, MBA, and other, more experienced researchers helped answer those questions, it was “agonizing,” Cohen says. “You’re making calls that affect people’s lives.”
They also were troubled by the ethics of having a placebo group: they needed those volunteers to run the trial, but what if AMX0035 worked? “It’s a very hard issue in a disease like ALS that’s so rapid and progressive and fatal,” Klee says. The open-label extension allows participants to take the drug as long as they wish; about 90 percent enrolled. “It’s really humbling,” Leslie says. “They’ve decided, ‘this is a drug that we want to keep taking.’”
By the time they launched the trial, the young Amylyx team was thoroughly invested in the ALS community. “Once you spend time with … the doctors and nurses and therapists, the patients, the families, you feel so compelled to want to help,” Klee says. “It’s a really tough diagnosis. The people who care for them are just saints.”
In the day-to-day work of a pharmaceutical company—responding to emails, working through study protocols—“you can certainly get a little bit detached from what the underlying goal is,” Leslie says. But when he meets patients, “the thing that is amazing to me is they’re so thankful for the work that you’re doing … that these companies and these researchers are taking their time to work to treat a condition that they have.” He adds, “It really does motivate you to try and figure out what your contribution can be.”
Cudkowicz has seen countless people die and dozens of trials fail since the 1990s. But she always picks herself back up. “I keep a little folder next to my computer of notes I’ve gotten,” she says. “My patients and the amazing people who participate in clinical trials would write to me and say, ‘don’t give up.’ If they can keep up good spirits and not give up hope, I’ll give myself an hour or a day to feel awful, and then jump right back in it.”
AMYLYX CONTRACTED WITH A biostatistics firm in Utah that specializes in neurodegenerative diseases to crunch the data from the 25 study sites. They expected the firm to unveil the results in early November 2019, but by the Monday before Thanksgiving they were still waiting. “We were getting a little bit impatient,” Leslie says. “It’s tough to do work and keep yourself busy when there’s something like that looming.”
Finally, as Leslie watched TV late that night, he got a call from Klee: the biostats group was ready to unveil the data in a webinar. Cohen was already asleep; he walked to the office, three blocks from his apartment, in his pajamas. There he says he joined Klee and Leslie around their conference table, with bottles of champagne ready to “celebrate the work that had gone into the trial,” no matter what the results.
As they set up a projector to watch the presentation on the wall, “I was shaking,” Cohen says. “You put all this time into it, and it comes down to this one phone call.” They knew right away the news was good. “You could hear the whole stats firm screaming,” he says. “In drug development most things fail, and they basically never see something actually work.”
Positive results are so rare in the world of neurodegenerative diseases in general and ALS specifically that even though Amylyx could at first only reveal that they’d met their primary endpoint, the slowing of disease progression, to a “statistically significant” degree, it was huge news. “It’s a hard endpoint to meet,” says Melanie Leitner, whose clients include the ALS Investment Fund and ALS Finding a Cure, both of which have supported Amylyx. She hasn’t seen the data, and says, “We’re super cautiously optimistic.”
“Any time a drug shows positive efficacy, it is time to be excited,” says Kuldip Dave, PhD, vice president for research at the ALS Association, which with ALS Finding a Cure helped fund the trial. He also hasn’t seen the data, and notes “ifs and buts” about the effect size and for which patients the drug worked. “I don’t want to reduce our enthusiasm,” he adds. “It’s a good group. … It’s exciting to see them get to this stage.”
Cudkowicz, who says she was “sitting down” when she got the results the next morning, says, “I’m beside myself.” It’s primarily good news for patients, she says, “but it also tells all the rest of the companies and academics working in the field that this is feasible. It draws in more companies, more funding, more options.” She continues, “I think this is just the beginning. This is going to be one drug, and then we’re going to see a cascade of drugs coming out.”
Anne Hart, of Brown, who wasn’t involved with the study, says “it looks encouraging,” even if it’s just one trial with a small number of participants. “I’m much more optimistic than when I entered the field about finding a cure,” she adds. “I’m pretty sure in the next 10 to 15 years we’re going to have something that will make a dramatic difference in patients’ lives.”
A few weeks after the unblinding, Cudkowicz threw a small party, where clinicians from the Healey Center told the Amylyx team “this was a positive day,” Klee says. “They got to tell their patients, ‘there’s something that might benefit, and we helped develop it.’ It was just really special to be a part of that.”
“One nurse told us that every day for the last two weeks, they’ve had somebody die,” Cohen adds. But that day, “it was a happy day, it was a hopeful day. She was like, ‘I don’t get those.’ We did what we did in developing the drug, but really the people taking care of these patients every day are heroes.”
AMX0035 IS NOW IN THE FDA’s hands. Amylyx has been working with the agency to set up a review meeting and find out what to do next. “Their feedback could guide us towards running a future trial, could guide us towards approval, guide us in some other way—I don’t know,” Cohen says. Klee points out that the FDA fast-tracked one of the only two drugs to treat ALS, edaravone, in 2017 based on a six-month trial in Japan that also, coincidentally, enrolled 137 people. “So we think there’s at least precedent,” Klee says.
Even as they await the FDA’s word, they’re scaling up. Cohen and Klee didn’t hire their second employee, after Leslie, until last year; now they’re filling about 100 positions, many in sales, but also in research and development, financial, analytics, human resources, and leadership roles. And they’re ramping up drug manufacturing, so they’ll be ready to go if AMX0035 is approved. “Every day lost trying to scale those things up potentially could mean a day patients don’t have the drug,” Cohen says. “We feel it’s critical to invest in those things, being fully aware of the risk we’re taking.”
“We want to work around the clock to advance any potential therapeutic,” says Paganoni, who, as a researcher and physician at the Healey Center and Spaulding Rehabilitation Hospital, has been PI or co-PI on several ALS clinical trials. “People living with ALS, their families, and their caregivers—they have no time to wait. … It’s our responsibility to try to move as quickly as possible.”
Leitner says that regardless of FDA approval, “I feel like they’ve already been successful. They’ve already run a really well-designed trial. They’ve already pioneered a number of new outcome measures and biomarkers, and provided a lot of resources to the ALS community in terms of samples and data.” She adds, “We will build upon it no matter what.”
In addition to building upon its work in ALS, Amylyx wants to expand its focus to other neurodegenerative diseases. Leslie is working with academic researchers to understand how their drug might be used to treat Parkinson’s or multiple sclerosis and to plan preclinical trials. And, finally, Cohen and Klee get to test the theory that launched Amylyx in a dorm room seven years ago: that combining PB and TUDCA could slow the progression of Alzheimer’s disease.
“We had put it on the back burner,” Cohen says, when they learned about a request for proposals for combination therapies that don’t target beta-amyloid or tau, two proteins whose misfolding and accumulation are implicated in Alzheimer’s. After winning nearly $2 million in joint funding from the Alzheimer’s Association and the Alzheimer’s Drug Discovery Foundation, in 2017, and additional support from the Cure Alzheimer’s Fund, Amylyx kicked off a 100-patient, phase two trial that finished recruiting earlier this year.
But ALS remains their priority. Klee says that while most companies at their stage would partner or sell, “We’re planning on doing this ourselves. This is a community that we’re fortunate that we’ve been a part of.” He adds, “We can really focus on patients with ALS, and thinking about how we can best serve them.”
Leslie says they want to do that not just by slowing ALS, but reversing it. “Let’s go back to the drawing board. What do we do next?” he says. “Sabrina and Merit are incredibly good at keeping you on task and reminding you of the reality that they see in the clinic every day.”
On his blog, Changing the Story, John Gerber writes eloquently about that reality, for himself as a caregiver and most of all for his wife, Phyl. “Watching her lose abilities has been a roller coaster,” he says in an email. But shock and sadness have given way to acceptance, he says, “based on a strong sense of the divine working in our lives.”
“We were very fortunate that just a few months after she was diagnosed, she was able to start the Amylyx trial,” Gerber adds. “Most of the people who developed symptoms at the same time as Phyl have passed. We are still going thanks to my wife’s stubborn will to live and Amylyx Pharmaceuticals.”