Can we remedy the digital malaise?
It started with a picture drawn by a 7-year-old girl. In brilliant color, she depicted herself and her happy family in a physician’s exam room. The doctor, though smiling kindly, is typing away at the computer, his back to the family.
The image was a wake-up call for the physician in the picture, Thomas Murphy, MD RES’12 F’15, and his colleagues at Rhode Island Hospital. Murphy was a pediatric resident at the time, a “very special resident,” according to Elizabeth “Betsy” Toll, MD, clinical associate professor of pediatrics and of medicine. He had already done a Navy internship and served two years as chief medical officer on an aircraft carrier of 2,500 people.
“He arrived, as an intern, a fully trained physician,” she says. “And yet, he was very humble, and very beloved by his colleagues, and his patients, and their parents. So along with the powerful message of this drawing came the sickening feeling: if this is how patients are looking at Tom Murphy, how are they seeing the rest of us?”
Toll was determined to find a way to share that picture and to get people to recognize how computers, and specifically the electronic health record (EHR), were intruding in the exam room. She wrote a reflective essay, called “The Cost of Technology,” that was published in the Journal of the American Medical Association in 2012.
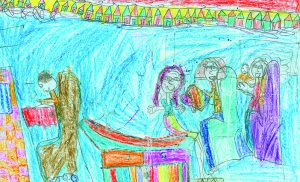
This drawing by a 7-year-old raised the alarm about the impact of computers on the patient-practitioner relationship. Courtesy Tom Murphy
That was exciting, she says, “but even more exciting was what happened afterward. People wrote from all over the United States and other countries like Argentina and Australia—doctors, nurses, lawyers, all kinds of medical professionals, most of them sharing my angst that their jobs had been stolen from them, and that they’d spent huge amounts of money to have this machine that doesn’t work well, that interferes with their ability to connect with their patients, the most meaningful and enjoyable part of their work.”
A few voices said it didn’t have to be that way, that physicians just needed to learn how to use the technology with the patient.
One voice belonged to Shmuel Reis, MD, an Israeli family physician, educator, and researcher on effective integration of technology in clinical care who has had a longstanding relationship with the Warren Alpert Medical School.
“We started a dialogue, and we had really diametrically opposite experiences,” Reis says. “As much as Betsy was in the angst of having to have a computer, I was already there in my 20-something year with computers in my practice, and I love my computer.”
Reis is part of a group of educators working on communication methods to use the computer effectively as part of the patient encounter “as an enabler, not a disabler,” he says. But the challenge is two-fold, as records systems used in the US are part of the problem, their design interfering and altering, wholesale, the work of the physician.
After communicating with others in the field who were thinking about and researching the topic, Toll and Reis decided there was a need for an entire conference devoted to how the electronic health record has affected the patient-practitioner relationship. In 2015, Allan R. Tunkel, MD, PhD, associate dean of medical education, gave them the green light to host an international conference at Brown, beginning an 18-month planning period with the support of Warren Alpert Medical School’s Office of Continuing Medical Education.
The payoff was “The Patient, the Practitioner, and the Computer: Holding on to the Core of Our Healing Professions in a Time of Technological Change,” a three-day conference held in March that brought together patients and practitioners—including physicians, nurses, nurse practitioners, medical assistants, and mental health professionals—as well as vendors and technology designers, health care stakeholders, and government officials from seven countries to study the impact of the EHR on the patient-practitioner interaction. Believed to be the first meeting of its kind, its goals were to open a dialogue among these stakeholders, determine what can and should be changed, and chart a course for getting there.
DATE NIGHT
In theory, the EHR sounds like a perfect idea. We all walk around with computers in our pockets anyway, so why not harness the technology in health care? Sharing medical records across systems, even competing ones, can improve patient safety and decrease duplication of care. With such potential, the federal government provided financial carrots to get providers to adopt EHRs, writing a $20 billion provision into the economic stimulus bill in 2009. The Health Information Technology for Economic and Clinical Health (HITECH) Act provided Medicare and Medicaid incentive payments to practices and hospitals that demonstrated “meaningful use” of EHR technology certified by the Department of Health and Human Services. Later, in 2015, the carrot became a stick: providers faced a reduction in Medicare and Medicaid reimbursement of 1 percent that increased each year that they did not demonstrate meaningful use of the technology, to a maximum of 5 percent.
According to the Office of the National Coordinator for Health Information Technology, by 2015, 87 percent of office-based physicians had some form of EHR. The same year, nearly all (96 percent) non-federal acute care hospitals had a certified EHR.
Indeed, the EHR hasn’t been all bad. Respondents on one panel at the conference were asked to list the unintended positive benefits of their system. They unanimously agreed on a few: patients have more information about their health because of access to patient portals driven by the EHR; practitioners can see other physicians’ documentation, noting their concerns, which helps with coordinating care; and, when properly designed and implemented, EHRs can actually save time, improve efficiency, and decrease administrative burden.
Hedy Wald, PhD, a member of the planning committee and an expert in physician resiliency and professional identity formation, saw the value of the EHR in patient education when she became the cancer caregiver for a family member. “The physician opened up the scans, showed us on the screen what was happening in the brain. It helped us understand so much better,” she says.
Negative consequences, however, have eclipsed the positive, and according to the literature, EHRs are spurring physician burnout and even driving some out of practice. According to a study by the American Medical Association, more than half of US medical doctors report symptoms of burnout such as emotional exhaustion and depersonalization. Burnout rose tenfold in three years—almost double the rate in the general population. Typically, higher levels of education are protective, but not so for physicians.
Christine Sinsky, MD, the AMA vice president for professional satisfaction, delivered the conference’s keynote lecture. A study she coauthored found that the major driver of professional dissatisfaction among physicians was the EHR. The chief complaint: “too much time per task.” She described a time-motion study published last year in the Annals of Internal Medicine that found that physicians spent a full 50 percent of the workday doing EHR and desk work.
And it’s not just the workday. Other studies have found that every hour of direct patient contact generates two hours of computer work. You don’t have to be a mathematician to predict what comes when the hours no longer fit in the prescribed workday: after-hours charting.
If Norman Rockwell were alive today, he might paint a tableau of the modern physician described by Betsy Toll. Every night, she and her husband, a pediatrician, get in their pajamas, build a fire, pull out their laptops, and chart across a card table from one another. “We’re empty nesters now, but I wonder, how are doctors with young children managing their work?” she says. “What kind of attention are their children getting?”
Ross Hilliard, MD RES’15, assistant professor of medicine (clinical), sees patients in the ambulatory clinic at Rhode Island Hospital and at University Medicine. He’s a certified physician builder on Epic, the nation’s second-largest health record system and the one used by Lifespan and Care New England. He says based on their usage data, they see some clear trends in EHR use.
“People are spending a lot of time outside of the office charting,” Hilliard says. “A look at our provider data shows us people are on the system as early as 4 a.m., then there’s what we call the ‘commuting dip’ between 7 and 8, and after that the system is active until 1 a.m.” On the ambulatory side, the only lull in usage occurs between 1 and 4 a.m.
Other studies have shown similar trends. “Saturday night belongs to Epic,” Sinsky said at the conference, noting one study that found system traffic peaks on the weekend.
One of the most lamented aspects of the electronic record systems is the endless checking of boxes. Sinsky worries that clicking through the tasks as prompted by the system leads to automation. “If we march through the visit in a generic way,” she said in her remarks, “we’ll start to see our patients as generic, and stop listening to their stories.” In her role at the AMA, Sinsky travels the country taking the pulse of the nation’s physicians. They tell her things like, “I became a doctor to take care of patients. I have become the typist.”
Those check boxes, Toll says, are not designed with the patient visit in mind, but to serve billing and regulatory systems. The number of checked items determines the level of reimbursement insurers will pay, or demonstrates compliance with Medicare regulations. Other regulatory-driven questions come from The Joint Commission, the state, and hospitals’ or practices’ own policies. And every little click adds up.
Shmuel Reis offers an international perspective. In Israel, where the electronic health record system was paid for by the government, the physician workflow is the driver. “They wanted people to be efficient. They wanted all the functions of prescribing, refilling, and documenting to be efficient and as few clicks away as possible,” he says. And in a single-payer health system, there are no insurance-driven questions.
“In my practice,” Toll says, “it takes five clicks to order one flu shot.” Studies have shown the average emergency room shift includes 4,000 physician clicks.
Interfaces that are not well designed are going to cause problems even for digital natives. Hilliard, who entered practice just as the transition from paper charts to EHRs was happening, says: “The biggest predictor [of problems]is how many clicks it takes to do something in the record. That’s going to be painful for anybody.”
Overly busy screens can lead to information overload. Toll uses the example of ordering prescriptions. Prescribing an antibiotic can involve searching through a long list of options to make the right selection. “What if I click the wrong one?” she says. Information processing like this increases cognitive workload.
TEXTING AND DRIVING
Reis says the problem isn’t just the EHR itself, it’s that practitioners are not learning how to use it in their communication with patients. They are not learning how to shift attention from the computer to the patient, in order to maintain eye contact. They are trying to multitask, in real time, with the patient watching.
“It’s like texting and driving,” Toll says. Continuously dividing one’s attention is damaging to the physician-patient relationship.
By design, patients were front and center at the Patient, the Practitioner, and the Computer conference. The planning committee, Toll says, wanted patients to be an integral part of the discussion, and included one on every panel. Most patients living with chronic conditions said they like the electronic health record because they feel it helps their doctors manage their complex care. One patient, Nicole Purcell, said during a stressful period in her life she had become less vigilant in caring for her type 1 diabetes. Sitting down with her doctor at the computer, and seeing her lab values in black and white, helped her get back on track.
But other patients report having less eye contact with their physicians makes them feel they do not have their full attention. The problem is not unique to the US: Reis says he hears it wherever he goes.
“Whenever I was traveling, and I was in a cab—whenever a cabby asked me what do I do, and I spoke about dealing with the computer in the exam room, invariably, cabbies all around the world said, ‘Oh, me, my daughter, my mother went to the physician, and they didn’t look us in the eye. They just look in the computer.’ So it was a realization that, worldwide, people and professionals are experiencing some damage, some issue when it comes to communication,” Reis says.
That’s the heart of the problem, according to Toll. Think about why people go into healing professions in the first place. “It probably has to do with healing parts of ourselves,” she says. “When you sit with patients and understand what’s going on with them and help them and they’re grateful, they, in turn, restore you.”
Toll adds, “And I think for people who entered this field with the need—whether conscious or unconscious—to be healed in the course of healing, it comes as a rude shock to find we’re spending our days in front of a computer screen.”
SHARE THE CARE
Though the three days of the conference offered plenty of time for venting, a number of sessions provided workable solutions to improve or stave off EHR burnout and use the computer to improve patient care. Suggestions ranged from the individual level to the practice level, to larger-scale change involving software design and regulatory agencies.
One ongoing theme was greater involvement of patients in their own care, ranging from increased patient-physician interaction through portals to patients having access to their own office notes. Practices also can move toward a team-care delivery model using medical assistants and nurses for documentation and wraparound patient care. It follows the adage “everyone working at the top of their license,” so physicians are doing the things only the physician can do, not documenting the visit, or doing billing and follow-up paperwork and calls. This is different from using scribes, who are simply documenting the visit.
Sinsky uses this model in her practice, and pointed out “that the delivery models of the future cannot be managed with the staffing models of the past. The ideal is two to three medical assistants or nurses per physician.” At first, she was concerned patients would be wary of having another person in the room, but in practice it has only enhanced relationships with patients. They appreciate having another person looking out for them, she said. And patients always have the option of not having the medical assistant present.
At the tech design level, practitioners asked vendors to listen to their concerns and to think about real practice issues, rather than trying to replicate paper charts in a computerized format. One vendor, Christine Tremblay, director of product strategy for Rhode Island’s Amazing Charts, said she wants next-generation records systems to incorporate machine learning and natural-language processing. That would free up physicians to document visits in a narrative rather than checkbox form.
Hilliard says health systems, too, need to involve practitioners in the adoption and development of their EHRs. “One of the things I was surprised to learn at the conference,” he says, “was that more places than I thought really don’t have providers at the table when making these decisions.” Both Lifespan and University Medicine included providers in the process, he says.
He adds, “And don’t just pick the most tech-savvy doctor, but maybe the least tech-savvy, too, to point out the painful and non-intuitive parts.”
AN OUNCE OF PREVENTION
At the Warren Alpert Medical School, using the electronic health record is part of the curriculum, thanks in part to work done by Wald, Reis, Paul George, MHPE ’01 MD’05 RES’08, assistant dean for medical education, and Julie S. Taylor, MD, MS, adjunct professor of family medicine. In 2014 they published a paper in Academic Medicine on teaching students how to enhance patient-centered care using the computer. The skills include positioning the patient, the practitioner, and the computer for optimal interaction; starting the encounter with the patient’s concerns; and verbalizing a shift to the computer. Advanced skills encourage the patient’s participation in building the chart, utilizing information from the chart for shared decision-making and to reinforce discussion as well as communicating a note to the interprofessional team.
Wald, a clinical professor of family medicine and director of Resident Resilience and Wellbeing for the residency programs in Child Neurology and Neurodevelopmental Disabilities at Boston Children’s Hospital, lectures around the world on physician resilience and well-being, the state of which she calls “a public health crisis.” In addition to the damage to physicians themselves, “it relates to patient safety,” she says, “and to patient satisfaction. Data show that more engaged doctors have higher levels of patient satisfaction.”
The answer is not to throw the EHRs out the window, however, nor is it to “fix the physician” alone. She advocates for organizations to cultivate a culture of resiliency in which leaders listen and respond to physicians’ concerns. “There is an organizational strategy to reduce burnout,” Wald says.
While no silver bullet was found in the course of the conference, just talking about the issues seemed to help. “There was a lot of creative energy and thinking about next steps,” Toll says. Since the conference she’s been reframing her thinking about the EHR. “Emotions are contagious. Patients are going to pick up on my attitude about the computer, positive or negative,” she says. She has been preparing for visits in new ways, engaging nurses more in care, and doing more teaching using the EHR.
Tom Murphy, who’s now a neonatologist in New Jersey, brought his patient’s original drawing to the conference. He told the crowd that his feelings about the picture have shifted. “It changed from a cautionary tale to a tale of hope,” he said. “That interaction and human connection will not be lost, just changed, so long as there are those of us who care enough to talk about these issues, who care enough to make these issues matter.”




