The 2023 Academic Symposium showcases student research in a new way.
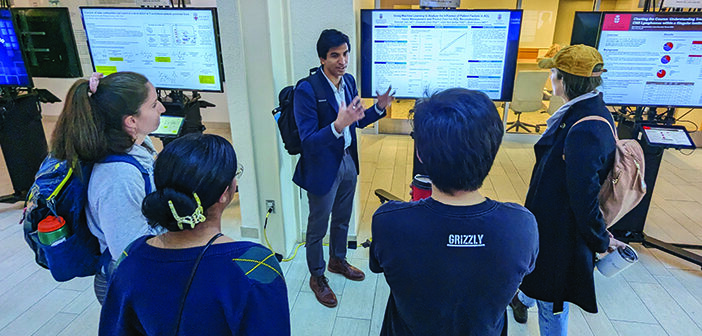
A new format for this year’s Academic Symposium at The Warren Alpert Medical School on Nov. 8 brought the student research experience alive digitally, as the Herbert M. Kaplan Atrium filled with screens, tablets, and students eager to share their presentations with their peers.
The 17th annual event featured a new approach to showcasing research, opting to drop the traditional poster boards that typically adorned the atrium during prior symposia. Julia Noguchi, director of community engagement and scholarship, said this was the first time the symposium has utilized digital screens for presentations. The change offered a more flexible and manageable experience—especially when considering that the change saved the printing of 130 posters.
“The students put an incredible amount of work into today,” Noguchi said. “The posters themselves are just a glimpse of the enormous effort that goes into the research itself.”
Methodius Tuuli, MD, the Chace-Joukowsky Professor and chair of the Department of Obstetrics and Gynecology, was this year’s keynote speaker, presenting “Towards Perinatal Health Equity: End of the Beginning.” Tuuli examined issues of equity compounding challenges with the national maternal mortality and morbidity rates, and some of the contributing factors. The US currently has the highest maternal mortality rates among high-income countries worldwide, at 23.8 deaths per 100,000 births, and Tuuli noted the “glaring disparity” with Black patients.
He emphasized the need to consider social determinants of health in creating health systems that provide equitable care. Tuuli cited community partnerships and a collaborative care model, which is also supported by health care services, like improved blood pressure monitoring and perinatal depression support services, combined with outreach initiatives like Meals on Wheels, to address some of the underlying psychological and social causes behind issues like hypertension.
“Most of life happens at home and in communities, and therefore it’s a big driver,” Tuuli said.
Among the student presenters this year was Franck Mbuntcha Bogni MD’26, who contributed to “Severity of Kidney Disease in an Aging population living with HIV in Rhode Island.” While novel combination antiretroviral therapy (cART) has improved mortality rates for those living with HIV, these patients are disproportionately affected by kidney disease. With the emergence of tenofovir alafenamide (TAF) regimens, the authors found a need to better understand the impact of specific antiretroviral regimens and the influence of gender, race, age, and other factors. Bogni and others pulled data from the HIV clinic at The Miriam Hospital, focused on patients ages 65 and up, and compared numerous characteristics, like whether they were on cART or TAF regimens.
“The major conclusion that we made here is that Black race and age were the sole independent variables that predicted the severity of kidney disease, and not the other variables,” Bogni said. “We didn’t expect whether you’re on the regimen or not to be a significant variable in this study. For it to be predominantly Black race is a little unexpected with the advances with health care and insurance policies. This tells us that we have a lot more work to do, as Black people in America are less likely to be insured or given the appropriate care they need.”
Bogni has a background in HIV research from his undergrad years, and participated in a postbac program at the NIH where he examined the immune system’s response to HIV infections. However, this topic holds personal significance.
“I also grew up in Central Africa, where there are a lot of cases of HIV, so that sparked my interest even as a young kid,” he said. “Coming to medical school was just a continuation of my work, which is more clinical and focused on how patients respond to therapies or side effects, and such.”
Nicole Comella ’19 MD‘24, a student in the Primary Care–Population Medicine Program, examined complementary and integrative health (CIH) therapies and barriers that prevent implementing them into health systems. CIH therapies include acupuncture, yoga, tai chi, and meditation, and account for $27 billion to $34 billion in out-of-pocket expenditures per year.
Her presentation, “Identifying Barriers to Implementing Complementary and Integrative Health in Health Care Systems,” involved interviewing administrators at health care systems, administrators at health insurance companies, physicians, and acupuncturists. She identified a number of underlying themes in their views on offering patients CIH, with major barriers being licensure issues and doubts of its validity or effectiveness.
Comella points to greater advocacy to increase access to CIH therapies, through processes like increasing insurance coverage, easing the process of credentialing providers, and further education and training.
“Also, these methods are very cheap—you can’t get a patent on acupuncture. There’s not going to be a lot of profit for hospital systems, so that is a huge disincentivization for these systems to offer them because they know they’re not going to profit from them as they would from a major surgery or a new drug,” she said.
Comella has had an interest in CIH since college and has a cultural background within her family using their own natural herbs or other things for healing. While in medical school she became certified in five- point ear acupuncture, and saw that patients benefited from it.
“We can talk about these things in a really wide scope, but there’s also a huge cultural value to including these things for patients,” Comella said.
Comella thanked Rani Elwy, PhD, professor of psychiatry and human behavior and director of the Brown Research on Implementation and Dissemination to Guide Evidence Use program, for her support and guidance.
“She quickly took me on as a mentee and has so much experience mentoring young researchers, so I gained a lot of important skills,” Comella said.
A number of students presented work produced as part of their scholarly concentration, an elective program through which Warren Alpert medical students undertake rigorous independent scholarship in a field of interest such as biomedical informatics, global health, or aging.
This year’s winners were:
Clinical Research: Weston de Lomba MD’26, “Risk Factors for Wound Complications in Prophylactic Paraspinous Musculocutaneous Flap Reconstruction of Complex Posterior Spinal Defects”
Basic Science: Patrick Barhouse MD’26, “Safety Profile of Silver Carboxylate as an Antimicrobial Coating: Viability and Mechanism in Human Cells”
Health Policy: Emily Wang MD’26, “The Effects of Climate Change on Marine-Related Health Threats in Rhode Island”
Medical Education: Maureen Whittelsey MD’26, “Healthcare Leadership Training: Medical Students’ Opinions and Curriculum Development”
Medical Humanities: William Choi MD’26, “Assessing the Canadian Public’s Attitudes Towards Medical Assistance in Dying for Patients who Refuse or Cannot Afford Medically Effective Treatments”