On the path to real impact in rare disease research.
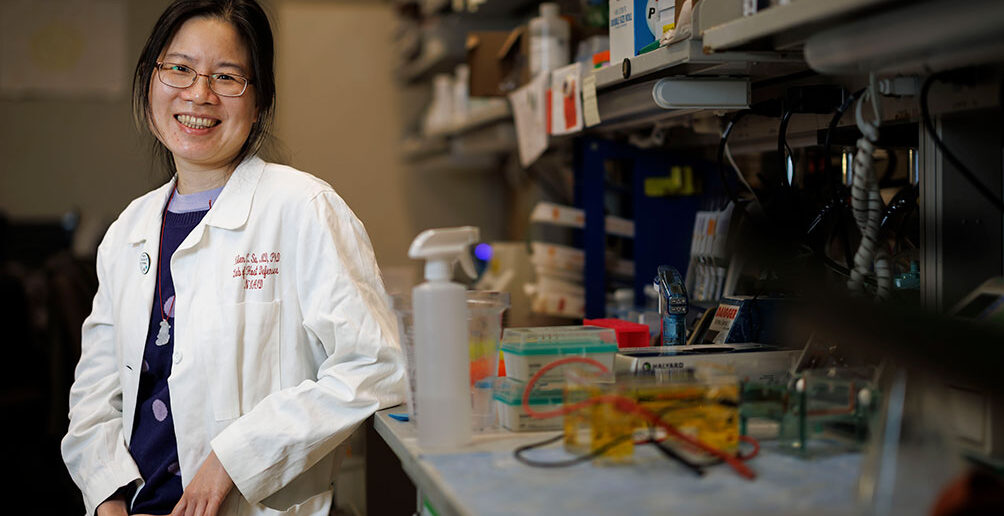
For Helen Su ’90 MD’98 PhD’98, learning to pose questions and tease out answers to them was shaped by both a “wonderful experience” at The Warren Alpert Medical School and some valuable input from Dr. Anthony Fauci himself.
Su, chief of the Human Immunological Diseases Section at the National Institute of Allergy and Infectious Diseases (NIAID), gained foundational knowledge of Q&A mechanics in the lab of the late Christine Biron, PhD, former chair of the Department of Molecular Microbiology and Immunology at Brown.
“I had to get confident enough to ask questions and solve them,” Su says. “It was a long process. I did not have an intentional path—I just followed my interests. It was not just about subject matter. Can I fit in this culture? Once I was convinced I could do both [MD and PhD], which specialty would allow me to pursue those interests?”
The small group in Biron’s lab embraced a collaborative atmosphere that enabled Su to find her next steps on that path. Su’s lab bench was next to Jordan Orange ’90 PhD’96 MD’97, P’23, who is now chair of the Department of Pediatrics at Columbia’s Vagelos College of Physicians and Surgeons.
“I was originally admitted into the second PLME class at Brown, as was Helen,” Orange says. “I had no idea about Dr. Biron. I found that lab during my second rotation. It was a phenomenal environment created by Christine. One of the benefits of diversity [in general]is we motivated and pushed each other in different ways.”
Both Su and Orange credit Biron, who died in 2021, as a mentor who made sure every student had a personalized path through Brown. “She devoted her life and career to Brown,” Orange says. “Christine had opportunities to be at many different places, and chose to be at Brown. She worked very hard to create individualized experiences before that was a thing. She was very proud of Helen and I.”
Su completed her pediatrics residency at Washington University and subspecialty training in allergy and immunology at NIAID. The culture at NIH proved to be beneficial for Su, who has family in Maryland. “I looked nationally, but NIH is a special environment,” she says. “The infrastructure allows you to see rare [disease]patients from throughout the US and abroad. They get great care.”
As a clinical fellow at the NIH, Su watched Fauci on rounds. “We would admit patients who have rare infections and [Fauci] would show up and ask questions,” Su says. “He was very to the point. There were some senior people who were quaking in their boots.”
The Human Immunological Diseases Section that Su oversees is focused on combined immunodeficiencies that lead to susceptibility to virus infections—including DOCK8 immunodeficiency syndrome. “We have DOCK8 deficiency research in the review process,” she says.
Making sense of massive amounts of data is time-consuming, but it’s a key element of providing treatment in the riskier projects the NIH takes on. “That is one of the bottlenecks,” Su says. “Science is increasingly more interdisciplinary. You have to be flexible, and lifelong learning is a necessity.”
Analyzing those rare diseases is an invigorating challenge that often leads to more data and more questions. “You have a girl with a rare disease who is really debilitated,” Su says. “How does that gene mutation affect her? This [effort]is so you can provide answers after they have exhausted everything. Hopefully, that leads to new therapies.”
Su and her colleagues provided those answers for a young woman named Whitney Ward, whose immunologist sent her case to the NIH in 2013. Three years later, the team delivered the news that a rare gene mutation caused her combination of autoimmune and immune diseases. Ward, a creative writer, shared her story in her 2021 memoir MORE Than My Mountains.
Su has relished seeing Ward’s journey through the last decade. “She has become much more self-assured,” she says. “Helping somebody makes this job fun.”
Now, finding the answers to questions posed in the lab has real impact. “You find a mutation and you find a drug that targets that mutation,” Su says. “It has been gratifying working on a long-term project for those patients.”