Stem cell models have been added to a biorepository for use by researchers.
Scientists at Brown University have developed an important new resource for the research community to help develop new treatments for CLN2 disease.
CLN2 disease is a rare genetic disorder that affects children. It is one of the most common forms of neuronal ceroid lipofuscinosis, a group of disorders also known as Batten disease. Children with CLN2 disease produce deficient levels of the enzyme tripeptidyl peptidase 1 (TPP1), which is involved in breaking down cell waste. Without enough of this enzyme, waste products accumulate in cells of the brain and retina, which subsequently contributes to loss of cognitive, motor, and visual functions.
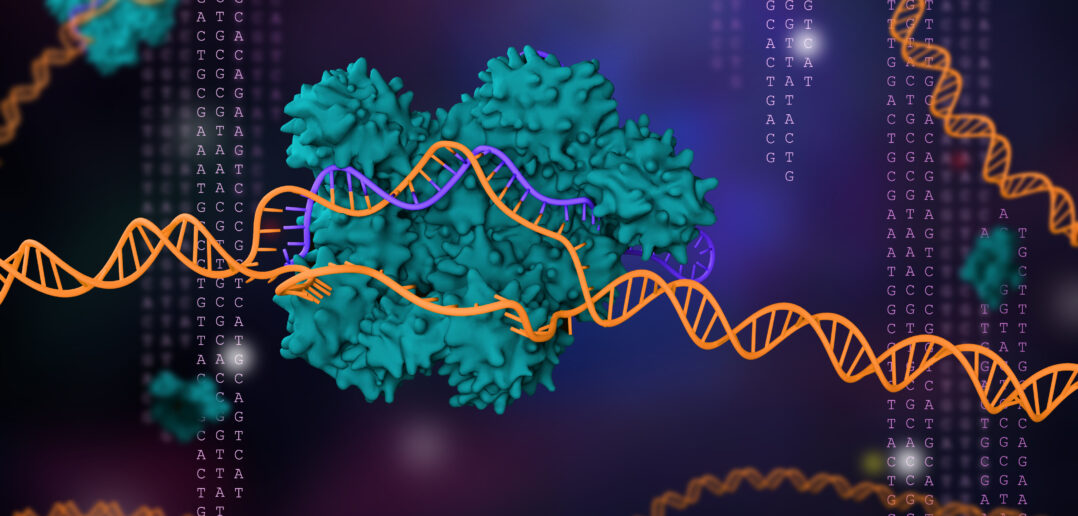
Eric Morrow, MD, PhD, a physician-scientist with expertise in childhood neurogenetic disorders, and his colleagues used CRISPR-Cas9 gene editing to introduce separately the two most common TPP1 mutations into human stem cells in the laboratory. These stem cells can then be converted into specialized cells, such as neurons, which scientists will be able to use to develop new treatments, including gene therapies for CLN2 disease, in the laboratory. CRISPR-Cas9 genome editing allows scientists to introduce specific sequence changes into the DNA of cells. The inventors of this powerful method that opened new opportunities in medical research received the Nobel Prize in 2020.
“We have combined two powerful methods—CRISPR-Cas9 genome editing as well as advanced stem cell biology—to build a resource for treatment development for CLN2 disease,” says Morrow, the Brown University Mencoff Family Associate Professor of Biology and director of the Center for Translational Neuroscience. He is making these newly engineered stem cell lines widely available to the research community by depositing them with the WiCell Research Institute (www.wicell.org) in Madison, WI.
“We hope that researchers will access these stem cells at WiCell so that we can move the research as quickly as possible to develop new treatments for children affected with this type of Batten disease and their families,” Morrow says. He and colleagues are sharing the cells prior to publication of a peer-reviewed paper. They have instead posted the manuscript describing how these cell lines were made to the open-access server bioRxiv. In this way, the information about the cells is available to other scientists that might be interested in using these cells for further CLN2 disease research.
More research on CLN2 disease is critically needed. Children born with this type of Batten disease typically develop normally at first. Between the ages of 2 and 4 years, children develop seizures, abnormal gait or problems speaking, giving families the first indication that something is wrong. From this point, the disease generally progresses rapidly, with most children losing the ability to walk, see, and speak by age 6 years. Symptoms tend to worsen as the disease progresses and children usually die between the ages of 8 and 12 years.
Currently, there is only one FDA-approved treatment for CLN2 disease—enzyme replacement therapy—that partially restores availability of the TPP1 enzyme. However, new treatments are still needed that can fully rescue TPP1 function throughout the brain and stop progression of the disease. Enzyme replacement therapies are also invasive: they require regular infusions of the enzyme directly into the brain and require a surgically implanted cerebral reservoir and catheter. Morrow’s new stem cell models of CLN2 disease can be used to develop various types of treatments, including gene therapy, which uses viruses to introduce healthy copies of the TPP1 gene into cells of CLN2 patients.
Generation of the CLN2 human stem cell models was made possible by the generous support of the Lehrman Family Research Fund, which said, “We thank Dr. Morrow and Brown University for developing these stem cell lines and we hope they will be widely used to develop new treatments for CLN2 Batten disease.”
References
Johnson TB, Cain JT, White KA, Ramirez-Montealegre D, Pearce DA, Weimer JM. Therapeutic landscape for Batten disease: current treatments and future prospects. Nature Reviews Neurology 15, 161-178 (2019).
Ma L, Prada A, Schmidt M, Morrow EM. Generation of pathogenic TPP1 mutations in human stem cells as a model for CLN2 disease. bioRxiv 2021.01.05.425495 [preprint](2021). Available from: https://doi.org/10.1101/2021.01.05.425495