“They’re dying now, but we are going to do something about this,” Charles Carpenter said about his patients at the dawn of the AIDS crisis. The Center for AIDS Research made his vision a reality.
On a distant continent, a virus from an animal infects a human, then most of a city. The virus continues to spread quickly, including to the West Coast of the United States. The disease it causes claims tens, hundreds, thousands of lives on almost every continent. The US president is slow to react. Anthony Fauci, MD, of the National Institute of Allergy and Infectious Diseases, will soon step up to help oversee the nation’s medical response to what has become a terrifying public health crisis.
No, it’s not January 2020, and the virus is not severe acute respiratory syndrome coronavirus 2. It’s 1982, and the CDC has just published the new term “acquired immunodeficiency syndrome,” which is caused by the recently discovered human immunodeficiency virus.
Forty years after the emergence of AIDS, and despite significant strides toward understanding and treating the disease, scientists have yet to find a cure. Since it emerged, HIV has infected 78 million people, and AIDS-related illnesses have killed 35 million worldwide.
To combat this deadly and enduring epidemic, in 1988 NIAID, part of the NIH, created the Centers for AIDS Research (CFAR), a program designed to foster innovative interdisciplinary AIDS research at academic research institutions. Ten years later, an NIH grant to The Miriam Hospital established a CFAR that was a partnership of Brown University, Tufts University, and Lifespan. Its founding director was infectious diseases legend Charles “Chuck” C. J. Carpenter, MD, who died in March.
While the strength of some CFARs lies in basic science, the Lifespan/Tufts/Brown CFAR focused on translational research and vulnerable populations right from the start. Drawing on Brown’s—and Carpenter’s—longstanding commitment to issues of social justice and on the medical and public health schools’ strengths in alcohol and addiction studies, the CFAR has been especially active in addressing the epidemic among marginalized populations—people in in the criminal justice system, individuals with substance use disorder, youth, and women. It was also one of the few CFARs to fund researchers employed by international institutions, beginning with India, the Philippines, and Ghana.
The center grew and thrived, but in recent years Tufts’ institutional support for HIV research (which is critical to maintaining NIH funding) waned. Then Boston University researchers approached colleagues at Brown hoping to form a CFAR, and the potential synergies and complementarities soon became clear. In 2018, the NIH awarded $9.1 million—its fourth five-year renewal grant—to The Miriam, and a new collaboration, renamed Providence/Boston CFAR, was born. Of the 20-some CFARs in the country, Brown’s is one of the few that have received continuous funding since their inception.
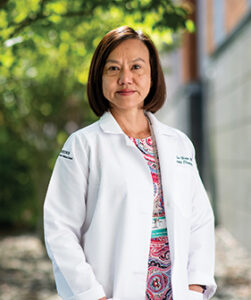
Susan Cu-Uvin succeeded Chuck Carpenter at the helm of the Providence/Boston CFAR. Photograph by Jared Leeds
Along with the impressive roster of academics that a large university provides, the new partnership significantly enlarged the physician and patient population. Boston Medical Center, BU’s teaching affiliate, is the largest safety net hospital in New England; the majority of its patients are from underserved populations, and it sees the vast majority of HIV patients in Massachusetts. BU also boasts the National Emerging Infectious Diseases Laboratory, or NEIDL, one of two National Biocontainment Laboratories in the country.
“BU and BMC strengthen our basic science research reach, as well as complementing our mission in underserved communities. So it was not a big sell to partner with us,” says Susan Cu-Uvin, MD, a professor of obstetrics and gynecology and of medicine at Brown and, since 2015, the director of the CFAR. “Their mission is very much the same as our mission.”
HOW CAN WE HELP?
The Providence/Boston CFAR supports emerging HIV investigators in many ways, including through its range of services, or Cores. The Cores make existing infrastructure and expertise available to anyone interested in doing HIV research. There are Cores for biobehavioral sciences, biostatistics, and basic sciences. Having easy access to a biostatistician or a psychiatrist with a deep understanding of HIV can strengthen a grant application, for example, and even redirect one’s line of inquiry. There are also administrative and developmental Cores, and a Community Engaged Research Council that connects the CFAR to the community it serves. Recently, as the opioid epidemic ravaged the HIV-infected population and put the HIV-negative population at risk for HIV, the CFAR added a Substance Use Research Core.
Working with researchers outside the field of HIV can yield interesting discoveries, says Andrew Henderson, PhD, a professor of medicine and microbiology at the BU School of Medicine and associate director of the Providence/Boston CFAR. “If you cross-fertilize with different technologies and ideologies, you can expand your thinking about the problem, you can expand the range of tools you can throw at it, and this might lead to new solutions and paradigms.” The Henderson lab has collaborated with BU bioengineer Wilson Wong, PhD, who makes molecules that mimic cellular responses, to gain insights into how HIV expression is controlled—in particular, how HIV persists and escapes the immune response.
PASS IT ON
Carpenter was prescient in perceiving the need to start training the next generation of HIV researchers now, Cu-Uvin says. “He didn’t think about today. He thought about tomorrow, and he harnessed the people who would answer the questions of tomorrow,” she says. “If he were a chess player, he would be three moves ahead of everybody.”
This forward-looking approach continues to animate Brown’s CFAR, which aims to cultivate the next generation by serving as both incubator of novel research and launchpad for young investigators’ careers. It does this in many ways, including through funding opportunities like the CFAR developmental awards.
Assistant Professor of Psychiatry and Human Behavior Laura Whiteley RES’11, MD, studies at-risk behaviors in adolescents and young adults, and how technology might help improve health-related behavior. She has been developing low-cost, easy-to-use, mobile interventions designed to encourage people to improve their prevention or treatment regimen for HIV and sexually transmitted infections. She applied for and received a CFAR developmental award that enabled her to run a small randomized controlled trial in which she tested the effects of a set of emails and texts containing publicly available HIV-prevention content that had been specifically tailored to Black, Hispanic, and LGBTQ youth—groups for whom rates of new infection are particularly high. Her results showed that those who received the messages took more precautions to prevent infection, including by having less unprotected sex.
Not only did her trial enable her to show “proof of concept,” Whiteley says, it also resulted in publication and teed her up to apply for NIH funding—and she now has three National Institute of Mental Health grants to her name. Two of them are exploring whether specially designed iPhone games can improve youths’ adherence to antiretroviral therapy (ART) and pre-exposure prophylaxis (PrEP), a once-a-day pill that has been shown to be 90 percent effective at preventing transmission of the virus in HIV-negative individuals. A third study, in Jackson, MS, is testing whether text messages can get Black men who have sex with men to start PrEP, a matter of particular significance since they are five times more likely than their Southern white counterparts to become infected.
Another advantage of a CFAR developmental grant, according to Whiteley, is that it’s a relatively small-scale undertaking that yields important results for the nascent researcher. “It was a low-pressure situation. I got mentorship. I was able to tweak things as I went along, and there wasn’t a ton of paperwork, unlike with the NIH. I was able to have this pure, fun, exciting research experience,” she says. “If it weren’t for CFAR and my CFAR mentors, I wouldn’t be a researcher.”

Sabrina Assoumou studies how clinicians can make it easier for their patients to get treatment. Photograph by Jared Leeds
Sabrina Assoumou RES’08, MD, MPH, an assistant professor of medicine at BU and an attending physician at BMC, seized the opportunity to apply for a grant to do a randomized trial implementing rapid HIV and hepatitis C testing in a drug detoxification center. The advantage of rapid testing over laboratory-based testing, the results of which can take days, is that the population in detox centers is often transient; by diagnosing patients on site, doctors can then connect them to the support they need, from health insurance to ART and to the medication that cures hep C. Assoumou went on to present her results at two
international conferences—and then parlayed them into a prestigious mentored K award, the NIH’s five-year career-development grant that lays the foundation for a successful career as an independent researcher.
“My preliminary data allowed me to show that I have a track record of working with these viruses and this population,” she says. It also gave her the question she wanted to answer next: why, when there’s a cure, do so few individuals follow up to get care after they’ve tested positive for hepatitis C? Thanks to her K award, Assoumou was able to return to the detox center and, over the course of two dozen hour-long interviews, ask patients just that.
“Research allows me to think a lot about why things aren’t happening the way I would like them to, and how I can make a difference,” Assoumou says. “My goal is to develop an intervention that will make it easier for patients to come into my office and get the treatment they need.”
According to Vicki Godleski, the center’s administrative director, the Providence/Boston CFAR has so far supported 155 rising investigators through the Developmental Grant Program, and the $5.5 million it has invested has resulted in more than $63.7 million in NIH funding. “We’re very proud of our return on
investment,” she says.
GREENHOUSE EFFECT
Also central to the CFAR are its mentoring programs, which Henderson says are essential to the future of HIV research. “We need fresh ideas and new energy,” he says. “Junior faculty always bring that to any problem. If we can bring excited, energetic, smart people toward the problem of curing HIV, that’s a positive.” The CFAR offers grant-writing workshops, which provide a forum in which junior faculty present ideas for proposals and get feedback from an interdisciplinary group of senior faculty, as well as Think Tanks, at which junior faculty present and get feedback on early-stage ideas for a CFAR developmental grant.
Recalling his own Think Tank experience, Jack Rusley ’03 MD’10, MHS, an assistant professor of pediatrics and an adolescent medicine specialist, says, “You’ve got something like 200 years of combined research and mentoring experience in one room.” Through another, six-month-long program, junior faculty receive mentoring as they prepare to apply for an all-important K award; once their proposal is ready, it undergoes a mock review by CFAR faculty.

Jack Rusley wants to help teens talk to their parents about PrEP. Photograph by Jared Leeds
Last May, Rusley received a K award to study an intervention aimed at helping sexual-minority teens talk to their parents about using PrEP. That’s no small matter, since HIV affects sexual-minority youth at a higher rate than many other ages and categories. The benefits he gained by availing himself of CFAR’s mentoring options planted the “seed” of his recent award, he says: “Those programs keep reinforcing each other, creating layers of support. There’s this built-in structure of all these people with a track record of mentoring. When you apply for this kind of grant, the NIH looks at your mentoring team. I felt so confident in mine, I never worried about that.”
Rusley stresses that his mentors did more than help him acquire research funding. Kate Guthrie, PhD, a professor of psychiatry and human behavior, is just one example of someone who, he says, “was invested in me as a researcher, but also as a person.”
Rami Kantor F’07, MD, a professor of medicine and an infectious diseases physician-scientist, embodies the CFAR’s next-gen mission. After being recruited to Brown in 2005, he applied for and received a developmental grant; in 2007 he became a core faculty member. Today he is co-director of the Basic Science Core.
FOLLOW THE NEED
Carpenter and his colleagues always recognized they were working in the smallest state in the union. The work researchers like Whiteley are doing in places like Mississippi and beyond are central to the mission of the Providence/Boston CFAR.
“At Brown, the culture has always been ‘Think outside the box, be relevant, work for your community.’ So why wouldn’t we go beyond our state boundaries to where the help is needed most?” Cu-Uvin says. Early on, Brown’s CFAR became the first in the country to do work in Jackson—and the need there has only grown, as the South now accounts for more than half of all new HIV infections in the United States.
Jun Tao, PhD, an infectious diseases epidemiologist and assistant professor of medicine (research), took advantage of all of the center’s career-development offerings, securing a CFAR grant to study a peer-driven intervention for PrEP uptake among Black and Latino men who have sex with men, followed by a K award from the NIH, also related to PrEP uptake. She then secured a supplemental grant through the Ending the HIV Epidemic initiative launched by President Trump in February 2019 to study disparities in HIV care and viral suppression among rural communities in Arkansas. Tao was the first CFAR faculty member to receive NIH funding for work in Arkansas, and the Providence/Boston CFAR is the only one operating there.
Less than three months after Trump’s initiative was unveiled in Washington, a tragic spike in HIV infections occurred half a world away, among children in Larkana District, Pakistan. Just days before, Fizza Gillani, PhD, the CFAR’s informatics director, an associate professor of medicine (research), and a native of Pakistan, had given a presentation about an HIV awareness project she was starting in a small clinic in Khyber Pakhtunkhwa province. In early May, doctors from the affected area phoned her to ask, “Can you guide us?”
“I asked my CFAR colleagues, ‘Are you ready to help some HIV-positive patients in Pakistan?’ They all said ‘yes,’” Gillani recalls.
Over the course of six Sundays, CFAR faculty sat at Gillani’s dining room table and delivered a series of webinars to doctors and medical students in Sindh, where the outbreak occurred. She also traveled to Pakistan with a group of Pakistani American physicians and met with the National AIDS Control Program there, as well as with Prime Minister Imran Khan. A plan to bring 10 HIV researchers, physicians, and program administrators from Pakistan to Providence for a five-day training program in April was foiled by the coronavirus pandemic, but Gillani says she hopes to convene the group in 2021. Meanwhile, her HIV/AIDS Communications Project in Pakistan is ongoing in the Providence/Boston CFAR.
PIVOT TO COVID
HIV investigators were positioned to tackle COVID-19 right out of the gate. And it’s not just infectious diseases specialists, Cu-Uvin points out: “It’s the public health people, the sociology people, the bio-behavioral people studying HIV and the opioid epidemic, or HIV in the prisons. Every marginalized population that is affected by HIV is also hit hard by COVID-19, because of structural inequities.” And, she says, if we are able to envision a vaccine taking less than two years to develop rather than 10, it’s because of decades of HIV infrastructure and training.
Many Providence/Boston CFAR faculty have incorporated COVID-19 into their ongoing HIV work. Henderson points to a proposed partnership in which CFAR investigators and the scientists in the NEIDL’s biosafety laboratories will study how SARS-CoV-2 initiates a cytokine storm (a hyperactive damaging immune response that is caused by the viral infection), and how the virus changes during the course of the disease.
Kantor, too, has added SARS-CoV-2 to his work, studying its genome as well as the impact of COVID-19 on people in Kenya. In April, he and Brown engineering professor Anubhav Tripathi, PhD, received support from a new University seed fund designed to fast-track research that directly addresses the COVID-19 pandemic; they plan to develop a molecular surveillance tool to monitor spread of the virus regionally and beyond, and to see if genotypic variants of the novel coronavirus affect patient outcome. Kantor recently published the first study of HIV/SARS-CoV-2 coinfection, in the Journal of the International AIDS Society. Katrina Byrd F’20, MD, an infectious diseases fellow and his mentee, was first author.
With 1.7 million new HIV infections worldwide each year, CFAR’s work is far from done. And given the devastation caused by the new pandemic, HIV research has an even more urgent salience. “We go where the problems are,” Cu-Uvin says. “We evolve. We want to provide the services that are most necessary in the current moment rather than what we needed five years ago.”