But Hollenbeck persevered. “You can hang in there,” she says. “You can laugh or go crazy.” She divorced and, with her children and her mother, moved across the country, to Seattle, where she worked for community health centers and group practices, as well as at the naval hospital in Bremerton, WA, where she taught residents. At home she found herself again caring for an aging parent, when her mother developed Alzheimer’s. But taking such responsibility is “in my bone marrow,” says Hollenbeck, who in 2001 flew her mother’s body home to Boston, to bury her. “There has to be someone who takes care of what needs to be done.” A few years later her second son enlisted in the Army and went to Iraq. “He wanted to do something bigger than himself, to do something that counts,” she says, “the way he saw I felt about medicine.”
Helping patients brought Hollenbeck fulfillment and fed her passion for her work. “People are endlessly fascinating,” she says. She tried to make them comfortable with honesty and clarity, delivering hard truths with a smile when she could. “There is no law against laughing in the doctor’s office,” she says. She loved to break the ice with her mother’s Irish sayings and her father’s German jokes. But she didn’t lose sight of the gravity and responsibility of her charge. “People know whether a doctor gives a damn,” Hollenbeck says. “Seeing a new doctor is like going on a blind date. … If the patient isn’t comfortable in that room with you, then he or she won’t tell you their story.”
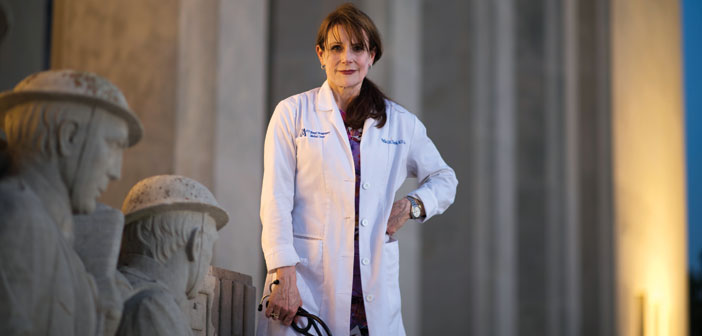
Her resolve turned out to be another requisite for the job. She has strong opinions on doctoring, and what she expects from herself and from other physicians as both their colleague and their patient. In the first chapter of her 2005 book, Sacred Trust: The Ten Rules of Life, Death, and Medicine, she writes: “I do not like doctors. Most of them, anyway. The two nicest sentences that have been uttered to me in my career are ‘You don’t look like a doctor’ and ‘You don’t act like a doctor.’” She recalls the many times a patient has told her, “You are so nice.” “Everybody should be nice,” she says. “Isn’t that just good manners? … It’s heartbreaking that people are so thankful to be treated with respect.”
Standing up for her patients, herself, and her staff to right wrongs was a matter of course throughout her career. “I have crossed swords with people,” Hollenbeck says. “I’m old enough that I’m not afraid to speak up.” In Sacred Trust she describes her mother as “five-foot-two, 115 pounds … [and]75 percent of that weight was due to her spine of steel.” Hollenbeck gained an inch on her mom, but she has that same backbone. “I’m bigger than I look,” she likes to say. “When people tell me I’m little, I always think they need their eyes examined.”
Administrators at the Jackson VA were hardly the first to underestimate Hollenbeck in her 37-year medical career, but they may have been the most hubristic. “They didn’t count on somebody as stubborn, as organized, who kept records,” she says. Siobhan Bradley, an attorney with the Disclosure Unit of the Office of Special Counsel (OSC), who has worked with many VA whistleblowers, says Hollenbeck’s meticulous recordkeeping assisted her case tremendously. “She had a lot of great information and supporting documentation. She’s very bright and very thorough,” Bradley says. “It was extremely helpful in organizing her allegations.”
From Seattle, Hollenbeck moved to northern Virginia to be with Sun, whom she married in 2008. His work, in private equity, brought them to Jackson later that year; the coincident primary care opening at the VA seemed serendipitous. Hollenbeck, of course, couldn’t have known the job was a revolving door. Nor could her superiors have known she wasn’t one more doctor they could push around. “Phyllis is such a wonderful patient advocate, so compassionate, that you expect her to be a bit more passive, a bit more willing to work within the system,” says Charles Sherwood, MD, a fellow whistleblower from the Jackson VA. “But when she perceived that things were wrong, that there was no sincerity on the part of leadership officials to rectify the situation, she became a force to be reckoned with.”
The imbalance among clinicians in the department was immediately evident to Hollenbeck; she soon was one of only three physicians, while up to 18 nurse practitioners were seeing most of the patients, unsupervised and incorrectly designated as licensed independent practitioners, and without identification tags indicating their professional title—contrary to VA policy and state law. “Nurse practitioners ran the place,” she says. “The nurse practitioner-physician ratio [in Jackson]is the inverse of other VAs. Most are three physicians to one nurse practitioner.” In her testimony before the House Committee on Veterans Affairs, in September 2013, Hollenbeck explained this concern was not just a matter of “protecting turf,” but of very different training and licensing requirements for physicians and nurses. “VA patients’ symptoms are getting more complex, and they need a physician to oversee their care,” she says. “You want the person who spent the most time being educated. Nursing is not where the buck stops.”
Meanwhile Jackson’s primary care physicians faced grueling schedules, with no control over the double booking and backlogs. “The more patients you see, the more orders, the more results to check and act on and notify people about—you had your heart in your mouth, praying not to miss something vital,” Hollenbeck says. She told the House committee that when she asked why she was always overbooked, she was told she saw her patients “too often.” Other patients were never seen at all; they’d been scheduled at “ghost clinics,” which had no assigned provider, and most would give up and leave, hours after their appointment time, and never receive treatment. “This is not fair to the veterans,” she says. “They signed up to put their lives on the line. And they’re supposed to come home and fight again?”
Even more egregious behavior was to come. After the hospital’s associate director of patient care services was charged with narcotics fraud, in May 2012 (the charges were later dropped), the DEA found that some nurse practitioners were improperly, and illegally, prescribing controlled substances, and stopped the practice. In response to what quickly became a crisis—Hollenbeck says leadership reported that 75 percent of veterans weren’t getting their narcotics renewed—hospital administrators began asking physicians to write prescriptions for patients they hadn’t treated. Hollenbeck refused. “You learn in the third year of medical school that you need to see the patient in order to prescribe narcotics,” she says. Both federal and state laws bar the practice, and Hollenbeck reported it to a local DEA agent. Yet the pressure to comply continued, under the guise of helping veterans and being a “team player.”