Though Hollenbeck’s supervisors sometimes verbally asked primary care physicians to order narcotics for patients they hadn’t seen, they also wrote the requests in emails, which she carefully saved, along with reams of other communications that documented the hospital’s many problems—the understaffing, the overbooking, the unsupervisednurse practitioners, the illegal prescribing practices—and years’ worth of messages she’d sent up the chain of command, voicing her concerns. By this time, she had visited her congressman’s office, where staff referred her to the OSC. The written requests to sign prescriptions were the last straw, she says. “I remember looking at the emails and thinking, ‘You stupid sons of bitches. I have you now.’”
Before veterans’ groups and the media became aware of the case, Sherwood says, the VA leadership “treated Phyllis and I and probably all the other whistleblowers as a disgruntled employee lunatic fringe. … They said we were well meaning, but we don’t have the big picture, it’s not as bad as we think. … But the OSC had other sources of information coming to them besides ours.”
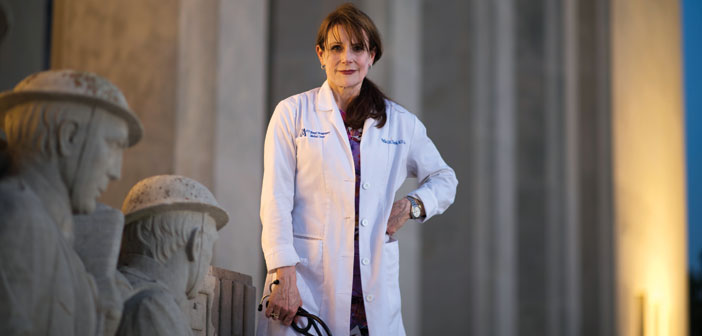
Sherwood, who retired from the Jackson VA in 2011 as chief of ophthalmology, went to the OSC last year with his allegations—regarding improper review of radiology images—at Hollenbeck’s suggestion. “She’s fearless,” he says of his former colleague. “She was running the gauntlet, still having to go to work every day and interface with these people in leadership. … She’s to be credited with taking great personal risk to see it through.”
Sherwood had witnessed retaliation at the hospital several years earlier, when he testified in the case of three female radiologists who had reported a colleague’s misconduct. In addition to pay discrimination, Sherwood says, supervisors made the women’s lives “a living hell for years.” But he believes Hollenbeck won’t suffer the same fate. “The size of the scandal made it possible for Phyllis to survive,” he says. “Whistleblowers are protected in ways they were never protected before, simply because of public awareness.”
Jose Mathews, MD, was not so fortunate. The former chief of psychiatry at the John Cochran Medical Center, in St. Louis, was removed from his position last year when he filed his complaints about scheduling problems, long wait times, and falsified data. After reading about Hollenbeck in The New York Times, last year, he contacted her; they speak regularly. “I knew that I was not alone and I got the encouragement to soldier on,” he wrote in an email. She put him in touch with the House VA committee, to whom Mathews testified in July about the need for more protections for whistleblowers. Until the OSC closes its investigation into his claims, however, it can’t help him regain his post. Meanwhile, the retaliation against him continues, he says. “I believe in the mission of the VA,” he wrote, but “the VA culture has NOT changed.”
Though the OSC strives to protect whistleblowers, coming forward “can be a risky endeavor,” says Nick Schwellenbach, the office’s senior communications specialist. “It has a huge impact on their personal and professional life. Some whistleblowers are fortunate and are in supportive environments, but too often they are not.” In July testimony to the House VA committee, Special Counsel Carolyn Lerner said her office was investigating 67 whistleblower retaliation complaints from VA staff.
Hollenbeck did not make the decision to go to the OSC lightly. She vividly remembers the moment when she finished writing and revising her statement and, on a Sunday night in July 2012, hit the “send” button. “I thought, it’s done. It’s too late to get it back,” she says. So accustomed to being ignored, she wondered if she’d hear back at all. Unbeknownst to her—the OSC keeps whistleblower disclosures confidential; Hollenbeck and Sherwood chose to go public—three other whistleblowers from Jackson had already come forward. Bradley called her that Friday, wanting to talk right away. To date, there are seven whistleblowers from the hospital; nationally, the OSC’s VA cases represent a quarter of its workload.
“I had sleepless nights. It took a lot out of me,” Hollenbeck says. “My husband is hugely supportive. You can’t do it alone. And without the two nurses and the clerk on my [primary care]team, I wouldn’t have survived. Every day we looked at each other and said, we can do this.”
When she testified before Congress, Hollenbeck spoke bluntly of the hospital leaders’ inadequacies and misdeeds, and called for their removal—“with management sitting there,” Sun points out. “So you know if they could find a way to retaliate against her, they would. … As long as she’s at the VA, and as long as those people or their cohorts are there, she has to act as if they would like to retaliate against her.”
Hollenbeck is still at the Jackson VA, though not in primary care. Shortly after her 35th reunion, she traveled to Houston for treatment of a serious illness. When she returned from medical leave, to the same crushing workload, she asked her supervisors— by then well aware, due to her copious messages, of the department’s staffing problems—to transfer her, on her doctors’ recommendation, to another office with a more predictable schedule. After getting no reply, she approached her congressman’s office with her allegations.
She got a new job—she now works in the compensation and pension office—but more gratifyingly, she helped expose a national scandal. Special Counsel Lerner cited Hollenbeck’s disclosures in two letters to President Obama, writing in June, “Too frequently, the VA has failed to use information from whistleblowers to identify and address systemic concerns that impact patient care.”
In response to that letter, the VA announced that it will restructure its Office of Medical Inspector, which Lerner criticized for downplaying or dismissing allegations that her office later confirmed. Medical facilities across the country are revamping their scheduling practices and reducing wait times. The new VA secretary, Robert McDonald, has vowed to overhaul the agency’s power structure, hire more clinicians, and “rebuild trust” with veterans and the public. Ongoing investigations by the VA’s Office of Inspector General into wrongdoings at dozens of medical facilities have confirmed that managers lied about scheduling problems and ghost clinics, and that such scheduling “schemes” were concocted to mask dangerous delays in care that may have led to patient deaths.
But problems continue in Jackson, Hollenbeck says, and she predicts more whistleblowers will come forward. “I believe we will eventually have such a tsunami of ethical physicians in the VA that the right culture change will happen—so many good and great people work in the system,” she says. She continues to work with the OSC herself, and to communicate her concerns to the highest levels of VA leadership. She insists that McDonald must meet with doctors who have stuck out the crisis and, playing on his previous post, as CEO of Proctor & Gamble, that he “wipe the slate clean.” She’s still calling for the heads of the leaders in Jackson whom she alleges are responsible for the problems there: “They’re very self satisfied. They still figure they’ll get away with it.” And she still goes to work every day, to help veterans, “the truest warriors”—to explain their benefits, hear their war stories, and comfort those who are dying.
It’s all part of the physician job description: a caretaker, by Hollenbeck’s definition, is a patient advocate. “A patient needs you to be able to say the things that need to be said. They count on you to stick your neck out,” she says. “I had to say something because it’s people’s lives. How many times can I say it? It’s a very simple mission: take care of the veteran.”