Indigo-derived drug shows promise in treating brain tumors.
A new study shows how a drug made from a natural compound used in traditional Chinese medicine works against malignant brain tumors in mice, creating a promising avenue of research for glioblastoma treatment.
In the study, published in Cell Reports Medicine, researchers also tested a new formulation of the compound, called indirubin, that was easier to administer, taking the potential pharmaceutical approach one step closer to clinical trials with human participants.
“The interesting thing about this drug is that it targets a number of important hallmarks of the disease,” says lead study author Sean Lawler, PhD, an associate professor of pathology and laboratory medicine. “That’s appealing because this type of cancer keeps finding ways around individual mechanisms of attack. So if we use multiple mechanisms of attack at once, perhaps that will be more successful.”
Glioblastoma is the most common and aggressive type of brain cancer. The standard of care is chemotherapy, radiation, and surgery, which may improve symptoms but don’t cure or stop the disease.
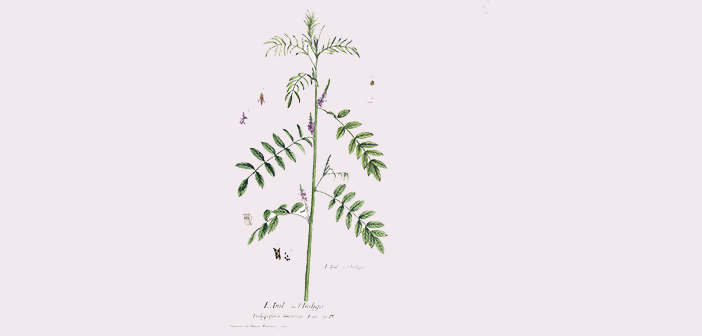
Indirubin is naturally present in indigo plants and a constituent of the traditional Chinese medicine Dang Gui Long Hui Wan, which has been used in the treatment of chronic myelogenous leukemia, according to the researchers. Derivatives of the indirubin have shown potential for the treatment of cancer through a range of mechanisms; Lawler has published previous research showing that indirubin slowed the growth of glioblastoma tumors in mice. However, he says, they weren’t able to explain why. What’s more, the modified drug wasn’t very easy to work with, making it challenging to test dosage levels or efficiently deliver it to the tumor.
For this study, the researchers tested a formulation of indirubin that is easier to inject on glioblastoma tumors in mice, focusing on how the drug would affect the immune system. Not only did it slow the growth and proliferation of tumor cells, but it also improved survival via effects on important immunotherapeutic targets.
“The drug impacted the immune system in these mouse experiments in a way that we think could enhance clinical immunotherapy in humans,” Lawler says.
The researchers will continue to test the drug to see how it interacts with chemotherapy and radiation, with the aim of developing clinical trials for people with glioblastoma.
“Over the past 20 years or so, there haven’t been many findings of note that have really impacted survival in a meaningful way,” Lawler says. “This research offers a new approach, and that’s why we’re so excited about it.”