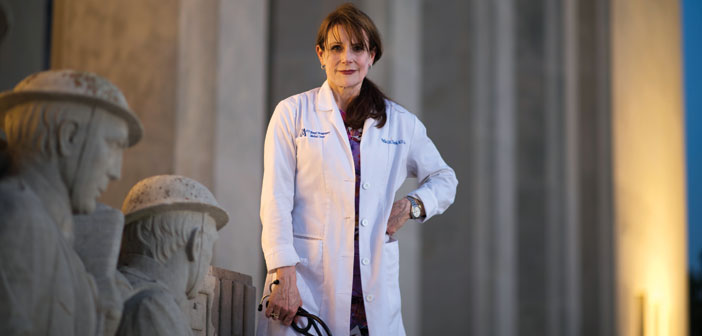
When she stood up for America’s warriors, VA physician Phyllis Hollenbeck had to become a warrior, too.
On her way to her 35th medical reunion at Brown, in May 2012, Phyllis Hollenbeck ’73 MD’77 got a call from a nurse on her primary care team at the G.V. (Sonny) Montgomery VA Medical Center in Jackson, MS. The US Drug Enforcement Administration had just arrested one of the hospital’s top administrators on narcotics fraud.
“You’re making this up,” Hollenbeck said to her colleague.
But Hollenbeck had long known that something was rotten in Jackson— indeed, had been wary since day one, in September 2008, when another physician welcomed her with, “I hope you don’t quit like all the others.”
It didn’t take Hollenbeck long to understand why. The primary care department was routinely overbooked, as the clinician ratio dwindled to six nurse practitioners for each physician; patients were scheduled with unsupervised nurse practitioners, or double booked and never seen. Unlicensed nurses prescribed medications, while physicians were asked to order narcotics for patients they’d never treated—which Hollenbeck refused to do, despite pressure from her superiors.
It was a pattern that was repeating itself at Veterans Affairs health care facilities across the country: long and falsified wait times, delays in medical care, illegal prescribing practices, and missed diagnoses, all so commonplace, and so callously ignored or concealed by leadership, that in the wake of the revelations last spring the VA secretary, Eric Shinseki, resigned. Rep. Jeff Miller, R-FL, chair of the US House Committee on Veterans Affairs, which has held multiple hearings to investigate the endless stream of wrongdoings, wrote of the “unprecedented specter of corruption” that “surpasses anything in the history of American government.”
In the summer of 2012, though, Hollenbeck didn’t know she was poised to play a key role in exposing a nationwide scandal; that she would receive federal whistleblower status from the US Office of Special Counsel; that she would testify, twice, before Miller’s House committee; that she would appear on nation-al television and on the front page of The New York Times.
She assumed the problems she witnessed were isolated to one dysfunctional department in one hospital of a sprawling medical system that cares for more than 6 million patients. And she thought she was standing alone when, at last, she approached the office of her US congressman, Gregg Harper, R-MS, to tell his staff of the impossible workload, its consequences for clinicians and patients, and her supervisors’ failure to act.
“They told me they were already hearing from veterans about primary care” at the Jackson hospital, Hollenbeck says. It was her first inkling that what she’d reported could have implications beyond her own day-to-day concerns,that this was bigger than her job and her patient population.
“I didn’t look for this fight—it came to me,” she says. “There is a firestorm now across the country. It’s wonderful.”